At NeuroVirt, our work is grounded in the science of neuroplasticity — the brain’s ability to rewire and recover through targeted, repeated movement. Every feature of our platform has been co-designed with clinicians, researchers, and patients to ensure it meets real clinical needs and supports meaningful recovery. By combining scientific rigour with lived experience, we’re creating XR tools that don’t just digitise therapy, but redefine how rehabilitation is delivered and experienced.
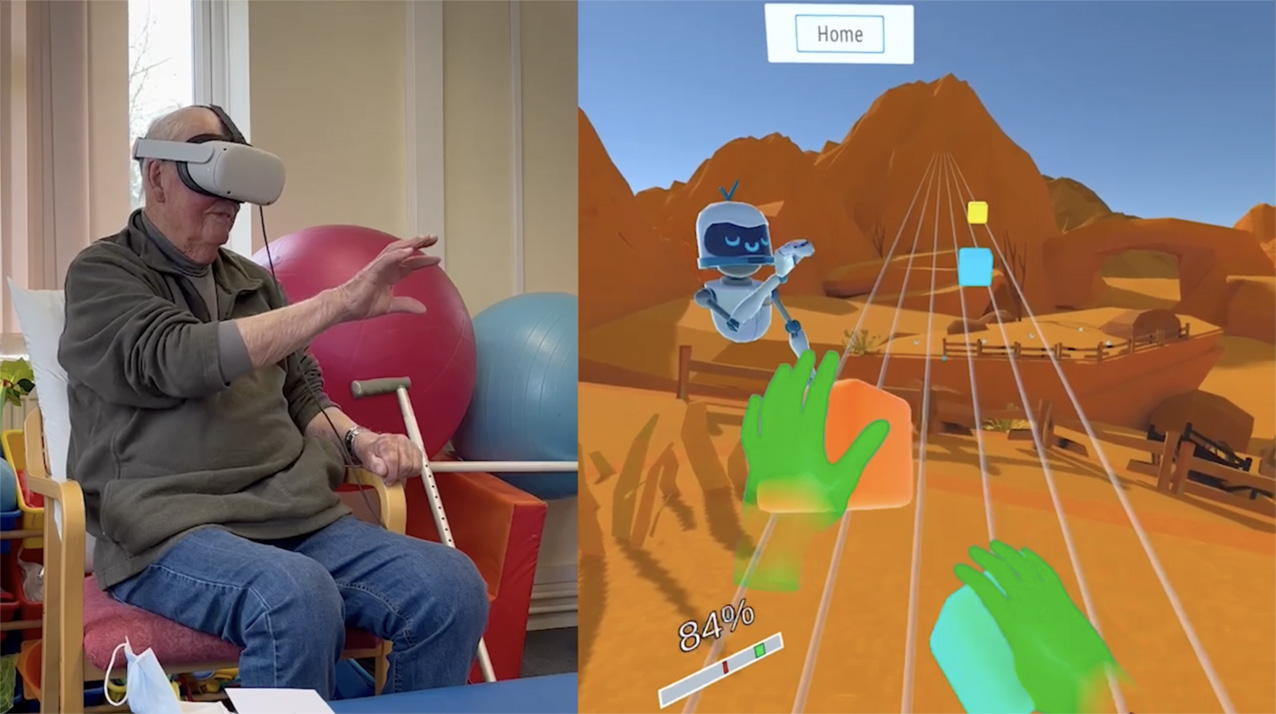
Intensive, high-dose therapy is crucial for effective stroke and neurological rehabilitation. Yet many patients receive insufficient rehabilitation dosage due to capacity or time-limited healthcare services and challenges with adherence to repetitive exercise. Neurotechnology can help increase motivation, engagement, and training intensity- key drivers of neuroplasticity. Since inception, NeuroVirt has been co-designed with patients and clinicians to create a patient-centred and accessible rehabilitation solution, using XR to enhance motivation and support better rehabilitation outcomes.
40 Stroke survivors were recruited from Hobbs Rehabilitation, Jan - Jun 2022. Each participant completed one NeuroVirt session. Participant feedback and therapist observations of sessions with clinical reasoning were recorded. Between sessions, NeuroVirt applied feedback for constant device development and improvement.

Co-design a clinically relevant neurorehabilitation device using immersive virtual reality

Test NeuroVirt's usability, tolerability and acceptability with subacute and chronic stroke survivors


You completely forget about what disability you have, it makes you realise that you can do more than what you think!
- Joyce,82 | Stroke Survivor





NeuroVirt continues to co-design with patients and clinicians. As of mid-2025, NeuroVirt it has been calculated that 500+ patients and 350+ clinicians have been involved in shaping NeuroVirt's tech
I was amazed at how well I could actually use my weaker limb, because I really haven't had the same amount of rehabilitation on my arm and shoulder as I would need. And I think this realy helped me a lot.
-MYRTLE
BRAIN INJURY Survivor
Clinical relevance was ensured throughout device development by regular clinician involvement. Stroke survivors effectively used NeuroVirt with good acceptance and tolerance. Case study results suggest NeuroVirt's potential for clinical efficacy as part of an intensive rehabilitation programme. Larger validation trials are required for generalisability.


Hayward, K. S., & Brauer, S. G. (2015). Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clinical rehabilitation, 29(12), 1234–1243. https://doi.org/10.1177/0269215514565395
Henderson A, Korner-Bitensky N, Levin M. (2007) Virtual reality in stroke rehabilitation: a systematic review of its effectiveness for upper limb motor recovery. Topics in stroke rehabilitation.14(2):52-61.
Ioannou, A., Papastavrou, E., Avraamides, M. N., & Charalambous, A. (2020). Virtual Reality and Symptoms Management of Anxiety, Depression, Fatigue, and Pain: A Systematic Review. SAGE Open Nursing. https://doi.org/10.1177/2377960820936163
Kiper, P., Szczudlik, A., Agostini, M., Opara, J., Nowobilski, R., Ventura, L., Tonin, P., & Turolla, A. (2018). Virtual Reality for Upper Limb Rehabilitation in Subacute and Chronic Stroke: A Randomized Controlled Trial. Archives of physical medicine and rehabilitation, 99(5), 834– 842.e4. https://doi.org/10.1016/j.apmr.2018.01.023
Lawrence E. at al., Estimates of the Prevalence of Acute Stroke Impairments and Disability in a Multiethnic Population, 2001. Department of Public Health Medicine. 32(1279-1284)
Mosadeghi, S., Reid, M. W., Martinez, B., Rosen, B. T., & Spiegel, B. M. (2016). Feasibility of an Immersive Virtual Reality Intervention for Hospitalized Patients: An Observational Cohort Study. JMIR mental health, 3(2), e28. https://doi.org/10.2196/mental.5801
Royal College of Physicians: Sentinel Stroke National Audit Programme (SSNAP), Cost & Cost effectiveness analysis, Technical Report, 2016. https://www.strokeaudit.org/Health-Economics.aspx
Worrall L et al., Reducing the psychosocial impact of aphasia on mood and quality of life in people with aphasia and the impact of caregiving in family members through the Aphasia Action Success Knowledge (Aphasia ASK) program: study protocol for a randomized controlled trial. 17(153) (2016). https://doi.org/10.1186/s13063-016-1257-9











